Fair use from OSHA
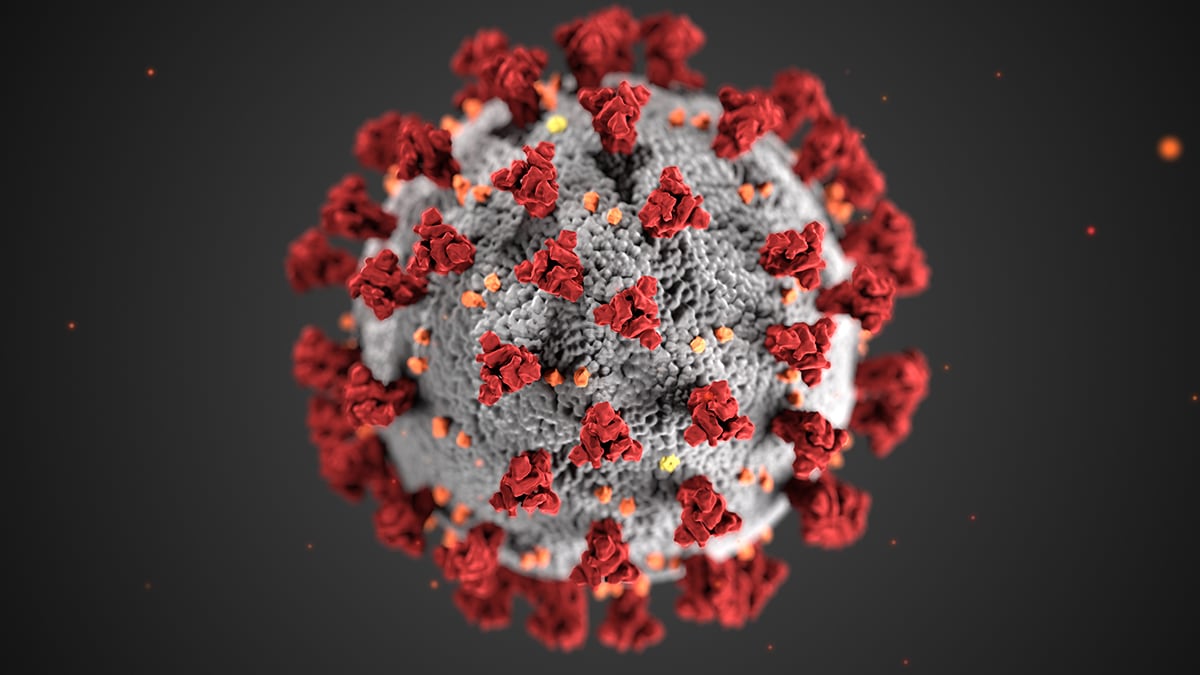
COVID-19
Healthcare Workers and Employers
This section provides guidance for healthcare workers and employers. This guidance supplements the interim guidance for U.S. workers and employers of workers with potential occupational exposures to COVID-19, above.
Until more is known about how the COVID-19 spreads, CDC and OSHA recommend using a combination of
standard precautions,
contact precautions,
airborne precautions, and eye protection (e.g., goggles or face shields) to protect healthcare workers with exposure to the virus.
CDC provides the most updated
infection prevention and control recommendations for healthcare workers managing suspected or confirmed cases of COVID-19.
Employers of healthcare workers are responsible for following applicable OSHA requirements, including OSHA's Bloodborne Pathogens (
29 CFR 1910.1030), Personal Protective Equipment (
29 CFR 1910.132), and Respiratory Protection (
29 CFR 1910.134) standards. See the
Standards page for additional information on OSHA requirements.
Engineering Controls
Engineering controls are the first line of defense in healthcare facilities to shield healthcare workers, patients, and visitors from individuals with suspected/confirmed COVID-19. This includes physical barriers or partitions in triage areas to guide patients, curtains separating patients in semi-private areas, and airborne infection isolation rooms (AIIRs) with proper ventilation.
Place patients with suspected or confirmed COVID-19 in an AIIR if available at the healthcare facility. AIIRs are single-patient rooms with negative pressure that provide a minimum of 6 air exchanges (existing structures) or 12
air exchanges (new construction or renovation) per hour. Ensure that the room air exhausts directly to the outside, or passes through a HEPA filter, if recirculated.
If an AIIR is not available, isolate the patient in a private room. Keep the door closed.
Isolation tents or other portable containment structures may serve as alternative patient-placement facilities when AIIRs are not available and/or examination room space is limited. Ensure that the room air exhausts directly to the outside, or passes through a HEPA filter, if recirculated.
The CDC/Healthcare Infection Control Practices Advisory Committee (HICPAC)
Guidelines for Environmental Infection Control in Healthcare Facilities contains additional information on negative-pressure room control for airborne infection isolation.
Administrative Controls
Consistent with the general interim guidance described above, isolate patients with suspected or confirmed COVID-19 to prevent transmission of the disease to other individuals. If possible, isolating suspected cases separately from confirmed cases may also help prevent transmission.
Restrict the number of personnel entering the room of a patient with suspected/confirmed COVID-19. This may involve training healthcare workers in appropriate use of PPE so they can perform tasks such as housekeeping and meal service to reduce the need for environmental and food service workers to enter areas where suspected or confirmed COVID-19 patients are isolated.
Follow CDC guidelines for
signs for and labeling of patient room doors when transmission-based precautions (i.e., contact and airborne precautions) are in place.
Minimize aerosol-generating procedures (AGPs), performing only those that are necessary for clinical diagnosis and care of a patient. Minimize the number of staff present when performing AGPs.
Safe Work Practices
Perform as many tasks as possible in areas away from a patient with suspected/confirmed COVID-19 (e.g., do not remain in an isolation area to perform charting; use closed-circuit television systems to communicate with patients in an isolation area when a worker does not need to be physically present).
Work from clean to dirty (i.e., touching clean body sites or surfaces before touching dirty or heavily contaminated areas) and limit opportunities for touch contamination (e.g., adjusting glasses, rubbing nose, or touching face with gloves that have been in contact with suspected/confirmed COVID-19 patients or contaminated/potentially contaminated surfaces). Also, prevent touch contamination by avoiding unnecessary touching of environmental surfaces (such as light switches and door handles) with contaminated gloves.
Ensure that there are systems in place to: differentiate clean areas (e.g., where PPE is put on) from potentially contaminated areas (e.g., where PPE is removed); handle waste and other potentially infectious materials; and clean, disinfect, and maintain reusable equipment and PPE.
Use caution when handling needles or other sharps, and dispose of contaminated sharps in puncture-proof, labeled, closable sharps containers.
Train and retrain workers on how to follow the established protocols.
Personal Protective Equipment
Healthcare workers must use proper PPE when exposed to a patient with confirmed/suspected COVID-19 or other sources of COVID-19 (See OSHA's PPE standards at
29 CFR 1910 Subpart I).
CDC and OSHA recommend that healthcare workers wear:
- Gowns
- Gloves
- National Institute for Occupational Safety and Health (NIOSH)-certified, disposable N95 or better respirators
- Eye/face protection (e.g., goggles, face shield)
Use respiratory protection as part of a comprehensive respiratory protection program that meets the requirements of OSHA’s Respiratory Protection standard (
29 CFR 1910.134) and includes medical exams, fit testing, and training.
When doffing potentially contaminated PPE such as a N95 respirator, do not touch the outside of the respirator without wearing gloves.
After removing PPE, always wash hands with soap and water, if available. Ensure that hand hygiene facilities (e.g., sink or alcohol-based hand rub) are readily available at the point of use (e.g., at or adjacent to the PPE doffing area).
Further Information
Emergency medical services (EMS) and medical transport:
- Workers and employers involved in EMS or other medical transport operations will likely need to adapt guidelines for the mobile work environment. That may mean relying on PPE (e.g., respirators) to protect workers when use of AIIRs or other isolation mechanisms are not practical and when staff have potentially prolonged, close contact with suspected or confirmed COVID-19 patients in transit.
Home care:
- CDC has developed interim guidance for healthcare providers who are coordinating the home care and isolation or quarantine of people confirmed or suspected to have COVID-19.
Cleaning and disinfection:
- Follow standard practices for high-level disinfection and sterilization of semi-critical and critical medical devices contaminated with COVID-19, as described in the CDC Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008.
- At this time, there is no EPA-approved list of disinfectants effective against COVID-19. EPA does not categorize disinfectants as hospital- or commercial-grade or keep a list of EPA-registered antimicrobial products registered for use in healthcare facilities. As a result, products effective at inactivating the virus must be determined based on data associated with inactivating similar or hardier (i.e., more difficult to inactivate) viruses. COVID-19 is a coronavirus and highly susceptible to inactivation by many commonly used disinfectants. Currently, OSHA recommends following SARS disinfection practices (see section D-10 in the linked document) for environmental areas contaminated with COVID-19.
The CDC advises the use of EPA-registered chemical germicides that provide low or intermediate level disinfection for SARS during general use (surface and noncritical patient-care equipment) because these products inactivate related viruses with similar physical and biochemical properties. CDC's
Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 provides information on the effectiveness of germicides on coronaviruses.
Deathcare Workers and Employers
This section provides guidance for deathcare workers, such as coroners, medical examiners, autopsy technicians, funeral directors, and other mortuary workers. This guidance supplements the general, interim guidance for U.S. workers and employers of workers with potential occupational exposures to COVID-19, above.
Until more is known about how the COVID-19 spreads, CDC and OSHA recommend using a combination of
standard precautions,
contact precautions,
airborne precautions, and eye protection (e.g., goggles or face shields) to protect mortuary and other deathcare workers with exposure to the virus.
Mortuary and other deathcare workers who have contact with the remains of people who have died from COVID-19 infection must be protected from exposure to infected blood and body fluids, contaminated objects, or other contaminated environmental surfaces.
Employers of mortuary and other deathcare workers are responsible for following applicable OSHA requirements, including OSHA's Bloodborne Pathogens (
29 CFR 1910.1030), Personal Protective Equipment (
29 CFR 1910.132), and Respiratory Protection (
29 CFR 1910.134) standards. See the
Standards page for additional information on OSHA requirements.
Prompt cremation or burial of the remains of individuals who have died of COVID-19 can help prevent worker exposure to the virus. (State and local requirements may dictate whether or not the remains of individuals who have died of certain infectious diseases can be buried or if they must be cremated.)
Follow recognized good biosafety practices to prevent or minimize transmission of infectious agents (i.e., COVID-19). To protect workers from COVID-19 exposure, OSHA recommends suspension of
post mortem or autopsy procedures on patients with suspected/confirmed COVID-19 infection. Although the infection process is not fully understood, this recommendation considers the potential for very high viral load (i.e., the number of viral particles in the body) at death and sources of exposure to workers performing autopsy procedures. If deemed necessary and appropriate, OSHA recommends strict adherence to basic safety procedures used for any autopsy on human remains, the general guidanceapplicable to all workers provided at the beginning of this page, and the controls described below.
Engineering Controls
Perform autopsies on remains of people who have died from COVID-19 infection in autopsy suites that have adequate air-handling systems. This includes systems that maintain negative pressure relative to adjacent areas and that provide a minimum of 6
air exchanges (existing structures) or 12 air exchanges (new construction or renovation) per hour. Ensure that room air exhausts directly to the outside, or passes through a HEPA filter, if recirculated. Direct air (from exhaust systems around the autopsy table) downward and away from workers performing autopsy procedures. CDC's
Guidelines for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings provides guidelines for AIIR use and recommendations for air exchange rates, which are similar to what should be followed in autopsy suites.
Section VIII - Infection Control for Laboratory and Pathology Procedures of CDC's
Infection Control in Healthcare, Home, and Community Settings for SARS also provides guidance applicable to pathology work, including autopsies, for coronaviruses.
Use a biosafety cabinet for the handling and examination of smaller specimens and other containment equipment whenever possible.
Equipment, such as saws, should be equipped with vacuum shrouds to capture aerosols.
Administrative Controls
Restrict the number of personnel entering the autopsy suite. This may involve training mortuary workers, such as medical examiners or autopsy technicians, to perform environmental services tasks (e.g., cleaning and decontamination) in lieu of additional workers entering such areas.
Minimize aerosol-generating procedures (AGPs), performing only those that are necessary to perform the autopsy or prepare remains for cremation or burial.
Minimize the number of staff present when performing AGPs. Exclude those who may be necessary for other procedures but not specifically the AGP.
Safe Work Practices
Follow standard safety procedures for preventing injuries to/through the skin during autopsy. Use caution when handling needles or other sharps, and dispose of contaminated sharps in puncture-proof, labeled, closable sharps containers.
Personal Protective Equipment
All mortuary workers and other deathcare workers who have contact with human remains known or suspected to be contaminated with COVID-19 must wear appropriate PPE (see OSHA's PPE standards,
29 CFR 1910 Subpart I). For workers performing autopsies, this includes typical autopsy PPE, such as:
- Double surgical gloves interposed with a layer of cut-proof synthetic mesh gloves
- Scrub suit worn under an impermeable gown or apron
- Goggles or face shield
- Shoe covers
- Surgical cap
Additionally, because of the sustained likelihood of aerosol generation during various steps of autopsy procedures, use respiratory protection as part of a comprehensive respiratory protection program that meets the requirements of OSHA’s Respiratory Protection standard (
29 CFR 1910.134) and includes NIOSH-certified disposable N95 or better respirators, medical exams, fit testing, and training. Powered, air-purifying respirators (PAPRs) with HEPA filters may provide increased worker comfort during extended autopsy procedures.
Remove PPE before leaving the autopsy suite and follow appropriate disposal requirements. After removing PPE, always wash hands with soap and water, if available. Ensure that hand hygiene facilities (e.g., sink or alcohol-based hand rub) are readily available at the point of use (e.g., at or adjacent to the PPE doffing area).
For other workers handling human remains:
- Wear nonsterile, nitrile gloves when handling potentially infectious materials.
- If there is a risk of cuts, puncture wounds or other injuries that break the skin, wear heavy-duty gloves over the nitrile gloves.
- Wear a clean, long-sleeved fluid-resistant or impermeable gown to protect the clothing.
- Use a plastic face shield or a surgical mask and goggles to protect the face, eyes, nose and mouth from potentially infectious body fluids.
- If there is a risk of aerosol generation while handling human remains, use respiratory protection as part of a comprehensive respiratory protection program that meets the requirements of OSHA’s Respiratory Protection standard (29 CFR 1910.134) and includes NIOSH-certified N95 or better respirators, medical exams, fit testing, and training. PAPRs with HEPA filters may provide increased worker comfort during extended autopsy procedures.
See the OSHA Fact Sheet,
Health and Safety Recommendations for Workers Who Handle Human Remains, for more guidelines to ensure worker safety when handling human remains.
Link to source:

www.osha.gov