I think that if H5N1 takes off and becomes Disease X - it won't be a scam. It'll be the real thing, possibly from GoF, or possibly the result of the destruction of the immune system from the mass vaccination for covid19. That being said - I agree with this article about the vaccine part.

As bird flu outbreaks spread among birds and mammals, the U.S. government says it has three FDA-approved H5N1 vaccines in its stockpile. However, experts questioned the effectiveness against current strains and raised concerns about potential side effects.

childrenshealthdefense.org
(fair use applies)
‘A Dangerous Vaccine for a Nothing Disease’: U.S. Stockpiling Bird Flu Vaccines
As bird flu outbreaks spread among birds and mammals, the U.S. government says it has three FDA-approved H5N1 vaccines in its stockpile. However, experts questioned the effectiveness against current strains and raised concerns about potential side effects.
By John-Michael Dumais
04/24/24
With the recent spread of H5N1 bird flu to dairy cows in eight states — and the infection of a Texas dairy worker marking the second known human case in the country — public health officials are raising concerns over the adequacy and safety of stockpiled vaccines meant to protect against a potential pandemic, according to Barron’s.
The Centers for Disease Control and Prevention (CDC) maintains bird flu is a low risk to humans — the infected dairy worker only contracted a case of conjunctivitis (pink eye) — and that there is currently no known mechanism for human-to-human transmission.
According to the World Health Organization (WHO), avian flu is responsible for 463 deaths worldwide over the past 20 years. The CDC reports only two U.S. cases of bird flu, and both were mild. No Americans have died from the virus.
Still, government agencies and Big Pharma manufacturers are building their capacity for bird flu vaccine production.
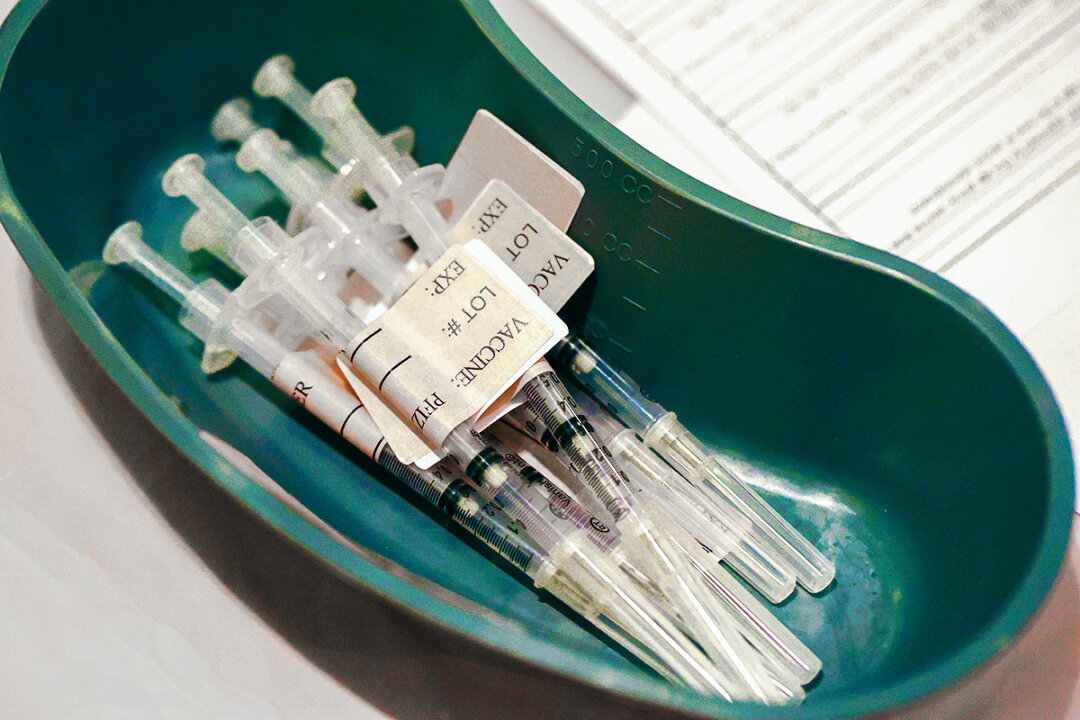
The U.S. government holds three U.S. Food and Drug Administration (FDA)-approved H5N1 vaccines in its National Pre-Pandemic Influenza Vaccine Stockpile.
The vaccines, manufactured by pharmaceutical giants Sanofi, GSK and CSL Seqirus, all contain mercury, a known neurotoxin, according to product inserts.
The same companies — plus Moderna — are working to develop new bird flu vaccines.
Federal officials said they supply several hundred thousand doses within weeks and 10 million more using materials on hand, and expect to produce 125 million doses within four months.
Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, suggested the agency has a “pretty low threshold” to deploy the stockpiled vaccines.
“We believe that, if we needed to, [our vaccines] would be reasonably good matches,” Marks said on April 1 at the World Vaccine Congress in Washington, D.C.
Given that all stockpiled vaccines were made for an earlier strain of H5N1, it’s uncertain how effective they would be against the strains that are circulating now, former FDA scientist Luciana Borio told STAT News.
“The FDA-approved H5N1 vaccines — licensed in 2013, 2017, and 2020 — do not elicit a protective immune response after just one dose,” Borio said. Even after two doses, “It is unknown whether the elicited immune response is sufficient to protect against infection or severe disease.”
A spokesperson for the U.S. Department of Health and Human Services’ Administration for Strategic Preparedness and Response (ASPR) program told Barron’s the agency could “ramp up production to make enough vaccine doses to vaccinate the entire U.S. population.”
A portion of the stockpile consists of “chunks” of premade antigens — good for training the immune system against specific strains — and adjuvants, the ingredients used to activate the human immune system when vaccines are administered.
However, despite its assurances of rapid vaccine delivery, ASPR did not detail its plans beyond claiming it could vaccinate about 68 million people, or one-fifth of the country’s population — using the two-dose regimen — within four months of an outbreak.
Internist and epidemiologist Dr. Meryl Nass, appearing with James Corbett on the April 20 episode of “Good Morning CHD,” said, “You’ve got a dangerous vaccine for a nothing disease,” noting the low number of human H5N1 cases reported thus far.
“It’s supposedly for a life-threatening illness,” she said. “Of course, pink eye is not life-threatening,” she said.
“The whole purpose of bird flu is to make you think the pandemics are out there, they’re coming for you all the time, and you need them [the health bureaucracy] to save you,” Nass said.
Sanofi vaccine contains thimerosol, PEG
Sanofi’s H5N1 vaccine, approved for adults in April 2007, was developed from a virus strain isolated from a Vietnamese patient in 2004.
“Our egg-based vaccine supply would well contribute to support a global influenza pandemic response should it arise either from A/H5N1 or any other influenza strain,” a Sanofi spokesperson told MedPage Today.
Each 90 microgram (µg) dose includes influenza virus hemagglutinin, 500 milligrams (mg) of porcine (pig) gelatin and approximately 98 µg of thimerosal, a mercury derivative (equaling approximately 50 µg of mercury/dose).
Other ingredients used in the development of the vaccine include embryonated chicken eggs, formaldehyde, polyethylene glycol and sugar.
Polyethylene glycol, or PEG, has been linked to the anaphylactic reaction in the COVID-19 vaccines.
The product warnings cited adverse events related to the 1976 swine flu vaccine, which included Guillain-Barré syndrome and other neurological disorders such as encephalopathy, optic neuritis/neuropathy, partial facial paralysis and brachial plexus neuropathy, as well as vasculitis and altered immunocompetence.
The initial clinical trial, conducted by the National Institute of Allergy and Infectious Diseases, featured an experimental group of 452 healthy adults ages 18-64, of which 103 were given two 90 µg doses administered 28 days apart, resulting in 44% of recipients developing a protective immune response.
The other adults in the vaccine group received 45 µg, 15 µg or 7 µg doses. The product information does not indicate their immune responses. However, given that the 90 µg/dose version is the one stockpiled, it’s likely the lesser amounts were ineffective.
Experts at the time expressed concern over the large doses, compared to the standard 15 µg dose used in seasonal flu vaccines, according to the Center for Infectious Disease Research and Policy at the University of Minnesota.
The trials didn’t include anyone under age 18, which would indicate that the safety and efficacy of the vaccine for this age group are undetermined.
GSK vaccine approved for 6-month-olds
GSK’s H5N1 vaccine, approved in 2013 for people as young as 6 months, was made from the same virus strain as Sanofi’s.
According to GSK’s package insert, each adult dose also contains the adjuvant AS03, made of 11.86 mg DL-a-tocopherol (vitamin E), 10.69 mg squalene (wrongly blamed for Gulf War syndrome, according to Nass) and 4.86 mg of an emulsifier called polysorbate 80. The insert also lists 5 µg of thimerosal, which equates to less than 2.5 µg mercury.
Other elements used in the production of the vaccine — and still present in the doses — include ovalbumin or embryonated hen eggs (at least 0.083 µg), formaldehyde (at least 12.5 µg) and sodium deoxycholate (at least 3.75 µg).
Pediatric doses contain about half the adult amounts of each ingredient, according to the product information.
In the clinical trial of about 2,000 adults 18 and older, 91% of those between 18 and 64 and 74% of those over 65 who received a two-dose (0.5 milliliters each) regimen of the GSK vaccine developed an adequate level of antibodies, according to the FDA.
The package insert warns of adverse events like Guillain-Barré syndrome, fainting and “cerebral vascular accidents” and notes one case of pulmonary embolism.
Three subjects developed thyroid cancer on days 21, 29 and 223 after administration. Two subjects developed polymyalgia rheumatica, two developed psoriasis, and one of each developed autoimmune hepatitis, celiac disease, cranial nerve 4 palsy, Crohn’s disease, facial paralysis and other symptoms.
A pediatric age group of 838 subjects ages 6 months through 17 years participated in a clinical trial. In addition to frequently reported symptoms of injection site pain, swelling, muscle aches, headache, fatigue, gastroenteritis, fever and other symptoms, serious adverse events included one report of a febrile convulsion and one case of alopecia within seven days of administration.
In a randomized control trial in eight countries outside the U.S. for children 6 months through 9 years old, one death was reported (day 42) along with one case of hepatitis and nasopharyngitis (day 385), three cases of appendicitis (on days 8 or 9) and one case of thyroid cancer (day 84).
Other adverse events included alopecia areata (2 subjects), glomerulonephritis (2 subjects), hypothyroidism (2 subjects) and idiopathic thrombocytopenic purpura (1 subject).
GSK recently said it could provide at least 200 million doses to governments worldwide in the event of a pandemic, according to Barron’s.
CSL Seqirus vaccine: 1 in 200 died during clinical trials
The most recent addition to the U.S. government stockpile of bird flu vaccines is CSL Seqirus’ Audenz for H5N1, approved in 2020 for infants and adults 6 months old and up.
The vaccine contains CSL’s MF59 adjuvant, which includes 9.75 mg squalene, 1.175 mg polysorbate 80, 1.175 mg of sorbitan trioleate, 0.66 mg of sodium citrate dihydrate and 0.04 mg of citric acid monohydrate.
Nass considers MF59 dangerous because it can stimulate autoimmunity. “This adjuvant has not been approved for most other vaccines,” she said. She noted that the FDA is willing to take more risks for a vaccine needed in a dire emergency.
Other ingredients from the production process include MDCK cell protein (at least 3.15 µg) and MDCK cell DNA (at least 10 nanograms), both from dog kidneys, cetyltrimethylammonium bromide (at least 4.5 µg) and ß-propiolactone (at least 0.1 µg).
Each 5 milliliter (mL) multidose vial contains 0.5 mL of thimerosal as a preservative, providing 25 µg of mercury per dose.
Fatality from the clinical trials included 11 (0.5% or 1 in 200) from the experimental group, compared to 0.1% or 1 in 1,000 for the placebo group.
In a trial with children ages 6 months through age 17, 8% of vaccine recipients developed upper respiratory infections within 21 days of vaccination.
Among the adverse events noted in post-marketing reports were swollen lymph nodes, swelling, anaphylaxis, Bell’s palsy, convulsions, demyelination, encephalitis and Guillain-Barré syndrome.
“So 1 in 200 died [and] you want to take this vaccine for a case of pink eye,” Nass said. “This is an example of how … one bad decision sort of goes and rolls down a hill and snowballs to another.”
New bird flu vaccines in development
As concerns mount over the effectiveness of stockpiled vaccines, pharmaceutical companies and government agencies are racing to develop new H5N1 vaccines better matched to currently circulating strains.
Barron’s reported that the U.S. government has been working with GSK, CSL Seqirus, Sanofi and Moderna to develop vaccines that better match the latest H5N1 strains.
GSK, recipient of multi-year pandemic preparedness contracts to supply a bird flu vaccine to the U.S., Canada, the European Union and the WHO, said it would be ready to supply 200 million doses globally, “updated with the latest circulating strains,” according to MedPage Today.
In October 2022, CSL Seqirus announced it was developing another vaccine based on the “pre-pandemic” H5N8 A strain, as part of ASPR’s Biomedical Advanced Research and Development Authority (BARDA) program.
The new vaccine also uses the MF59 adjuvant.
One of the surface proteins of H5N8 is reportedly similar, according to Barron’s, to the strain of H5N1 that infected the Texas dairy worker.
According to MedPage Today, CSL Seqirus said it could scale up production at its California facility — built in a private-public partnership with BARDA — to deliver 150 million vaccine doses during an outbreak.
Sanofi also partnered with BARDA in 2019 to “expand pandemic influenza preparedness” using the same recombinant technology as Sanofi’s Flublok Quadrivalent vaccine. Leveraging its existing technology would allow the company to more rapidly deliver a pandemic vaccine.
Moderna said in March 2023 that it planned to develop a bird flu vaccine, stating its COVID-19 vaccine was developed from its H10N8 pandemic flu vaccine research. Moderna didn’t mention the bird flu vaccine in its March 2024 announcements.
However, the company reported on its seasonal flu vaccine, mRNA-1010, saying it had “demonstrated consistently acceptable safety and tolerability across Phase 3 trials.”
“Early studies done by mRNA vaccine companies on seasonal flu are promising, which could be good news here since mRNA vaccines can be made more quickly than vaccines using eggs or cells,” said Borio.
‘Why is it called a biodefense project?’
Linking to a 2023 Global Biodefense article discussing BARDA’s work with CSL Seqirus, Dr. Peter McCullough tweeted on April 23, “Why is the bird flu (highly pathogenic avian influenza, H5N1) human vaccine a US @NIH @BARDA project with CSL? Why is it called a ‘biodefense’ project?”
The Daily Mail raised similar concerns about the U.S. Department of Agriculture (USDA) collaborating with the Chinese Academy of Sciences — which oversees biodefense labs like the Wuhan Institute of Virology — to develop more virulent strains of bird flu viruses, ostensibly to aid in the development of vaccines.
The White Coat Waste Project disclosed details of the USDA-China program in a February post showing numerous research project agreements beginning in April 2021.
A bipartisan group of Congress members on April 12 sent USDA Secretary Tom Vilsack a letter stating, “This research, funded by American taxpayers, could potentially generate dangerous new lab-created virus strains that threaten our national security and public health.”
Dr. Richard Bartlett, an emergency room director and former Texas Department of Health and Human Services advisory council member, in the April 10 episode of “The Defender In-Depth,” suggested gain-of-function research on bird flu viruses may be responsible for the current outbreak or could cause a future pandemic.
“After everything we just experienced and all the loss of life and bankruptcy and damage to the economy, families destroyed with COVID, why would you continue gain-of-function research?” he asked.
Nass told Corbett she was skeptical of the push for bird flu vaccines. “Every single time we’ve had an emergency and vaccines have been rolled out quickly, it’s resulted in disaster,” she said.
Nass cautioned against relying on centralized solutions pushed by public health authorities.
“They want you only to be able to get the solution they have made for you,” she said. “They don’t want it widely distributed where you have agency to decide whether you want it for yourself or not. … Don’t be scared. This is a scam.”